Celiac disease (CD)

Celiac disease: Pathogenesis
It is clear that the autoimmune celiac disease is a reaction to the gluten protein. But what triggers this disease? Celiac disease is caused by a complex pathology resulting from the interaction of genetic and exogenous factors.
Genetic factors in celiac disease
A high incidence of celiac disease of 10-15% among first-degree relatives and around 50-75% among monozygotic twins suggests a genetic contribution to the pathogenesis. An important genetic factor is the human leukocyte antigen system (HLA system), a gene complex whose task is to recognize foreign molecules. Approximately 90% of people with celiac disease carry the HLA-DQ2 trait, and almost all of the rest express the HLA-DQ8 gene. Although the presence of both gene complexes is necessary for the disease to develop, they are not solely responsible for it. However, these genes are also found in more than 30-40% of the healthy population.
Exogenous factors in celiac disease
The only exogenous factor known to date that plays a role in celiac disease is gluten, a collective term for the storage proteins found in wheat, rye, and barley. These proteins have a high proportion of proline and glutamine residues and are called prolamins. Wheat prolamines include gliadins (α, γ, and ω gliadins) and glutenins. They cannot be completely broken down by stomach and pancreatic enzymes and trigger the adaptive immune response in celiac disease.
Research is currently investigating whether and to what extent additional environmental factors—such as infections and the amount of gluten consumed, together with changes in the gut microbiome—play a role in the development of the disease.
Pathophysiology of celiac disease
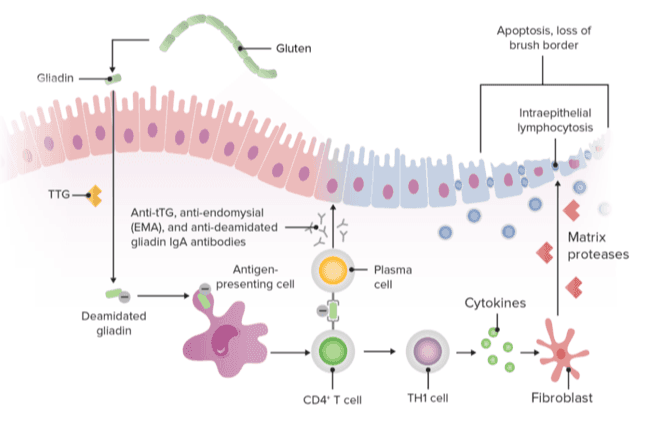
Gluten is usually consumed in large quantities (10-20g) in the normal diet. Some of the gluten peptides are not properly broken down by the stomach and pancreatic enzymes and are absorbed trans-epithelially via the lamina propria (small intestine mucosa).
Transglutaminase (TG2, also known as tissue transglutaminase) deamides gluten peptide residues, resulting in better binding to HLA-DQ2 or HLA-DQ8 on antigen-presenting cells (APCs) and potentiating the inflammatory response.
TG2 also facilitates molecular cross-linking, leading to the formation of TG2-gluten complexes. This activates:
- T lymphocytes with the release of cytokines and tumor necrosis factor alpha (TNF-alpha).
- B cells with the release of antibodies (anti-tTG and anti-gliadin antibodies).
- Cytotoxic lymphocytes, which interact with intestinal epithelial cells, contributing to tissue destruction and small intestinal atrophy.
Dr. Schär Institute Newsletter
Bundled gluten-related disorders (GRDs) expertise for your practice: our newsletter keeps you up to date on celiac disease and related topics.
Related topics you may find helpful

How to successfully diagnose celiac disease in practice
Read more
Treating celiac disease means educating, caring for and motivating people
Read moreSources
- Catassi C, Verdu EF, Bai JC, Lionetti E. Coeliac disease. Lancet. 2022 Jun 25;399(10344):2413-2426. doi: 10.1016/S0140-6736(22)00794-2. Epub 2022 Jun 9. PMID: 35691302.
- Gatti S, Rubio-Tapia A, Makharia G, Catassi C. Patient and Community Health Global Burden in a World With More Celiac Disease. Gastroenterology. 2024 Jun;167(1):23-33. doi: 10.1053/j.gastro.2024.01.035. Epub 2024 Feb 1. PMID: 38309629.
- Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet. 2018;391(10115):70-81
- Wieser H. Chemistry of gluten proteins. Food Microbiol 2007; 24: 115–19
- Sollid LM, Qiao S-W, Anderson RP, Gianfrani C, Koning F. Nomenclature and listing of celiac disease relevant gluten T-cell epitopes restricted by HLA-DQ molecules. Immunogenetics 2012; 64: 455–60.
- Pes GM, Bibbò S, Dore MP. Coeliac disease: beyond genetic susceptibility and gluten. A narrative review. Ann Med. 2019 Feb;51(1):1-16. doi: 10.1080/07853890.2019.1569254. Epub 2019 Mar 11. PMID: 30739507; PMCID: PMC7857446.
- Sharma N, Bhatia S, Chunduri V, Kaur S, Sharma S, Kapoor P, Kumari A, Garg M. Pathogenesis of Celiac Disease and Other Gluten Related Disorders in Wheat and Strategies for Mitigating Them. Front Nutr. 2020 Feb 7;7:6. doi: 10.3389/fnut.2020.00006. PMID: 32118025; PMCID: PMC7020197.
- Iversen R, Sollid LM. The Immunobiology and Pathogenesis of Celiac Disease. Annu Rev Pathol. 2023 Jan 24;18:47-70. doi: 10.1146/annurev-pathmechdis-031521-032634. Epub 2022 Sep 6. PMID: 36067801.
- Verdelho Machado M. Refractory Celiac Disease: What the Gastroenterologist Should Know. Int J Mol Sci. 2024 Sep 26;25(19):10383. doi: 10.3390/ijms251910383. PMID: 39408713; PMCID: PMC11477276.
