Celiac disease (CD)

How to successfully diagnose celiac disease in practice
Over the last 50 years, advances in the diagnosis of celiac disease have correlated with a steady increase in the number of medical diagnoses. Nevertheless, gluten-sensitive enteropathy is still underdiagnosed: 2 out of 3 people affected do not know that they have celiac disease (formerly known as indigenous sprue).
Who should be tested for celiac disease?
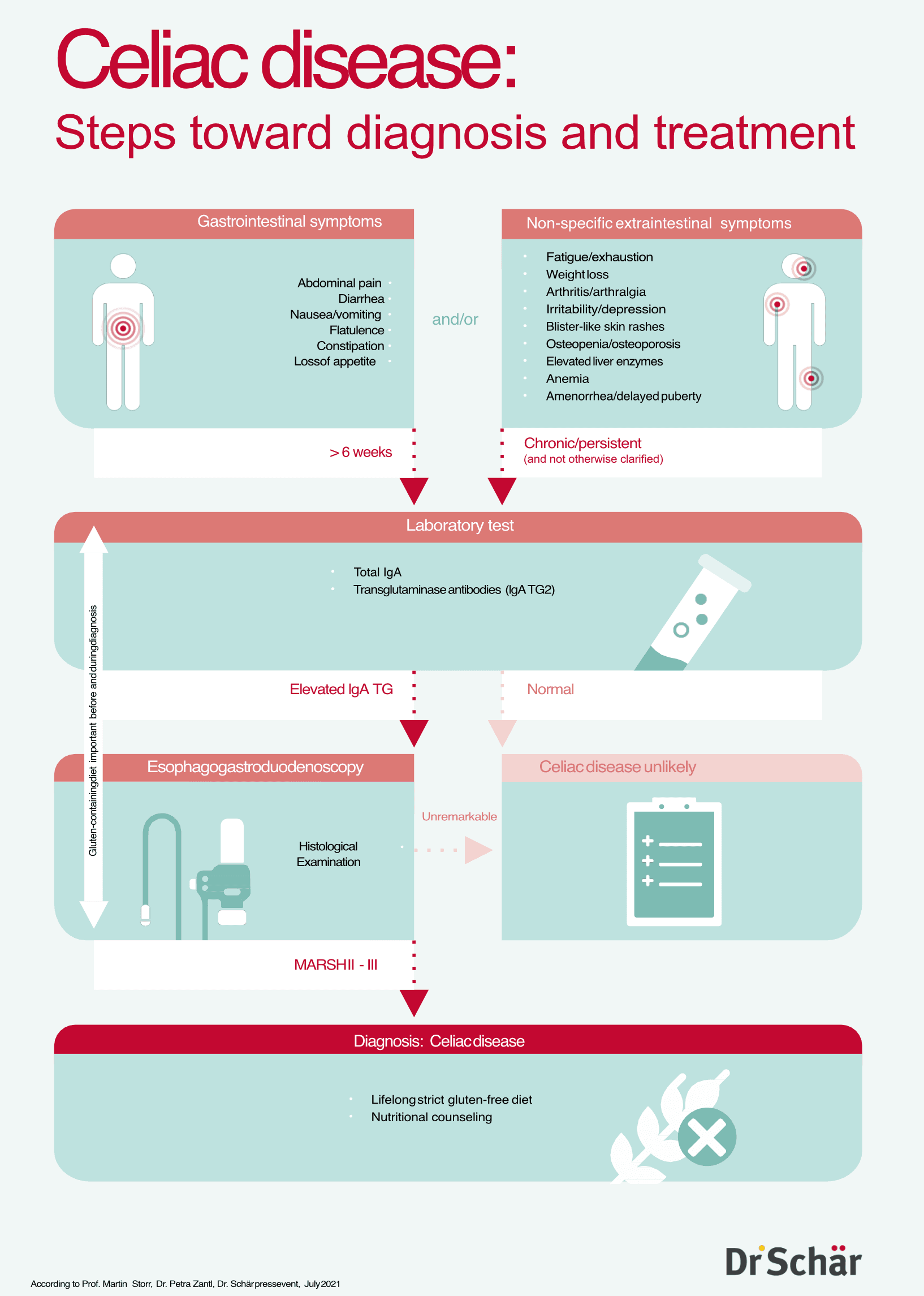
The autoimmune disease celiac disease is considered a "statistical iceberg". If we want to melt this in practice, the first hurdle is to identify those patients in whom laboratory tests for celiac disease are indicated. Serological gluten intolerance diagnostics are recommended for all those with an increased risk of celiac disease - and for anyone with suspicious symptoms Gluten-sensitive enteropathy can manifest itself gastrointestinally and extraintestinally at any age in a wide variety of symptoms or initially remain asymptomatic. The current guidelines for the diagnosis of celiac disease therefore strongly recommendthat testing for celiac disease be conducted in many different cases.
What should be considered before diagnosing celiac disease
Patients should definitely continue to eat gluten-containing foods before undergoing testing to confirm or refute the celiac disease diagnosis, so as not to falsify the results. If those affected have already reduced gluten in their diet, they should consume around ten grams of gluten per day in their diet for three months before the tests, which corresponds to 100 grams of uncooked pasta or 100g of wheat bread, for example.
Which celiac disease laboratory values should be checked
The first step in diagnosing gluten intolerance in practice is a simple blood test. In people suspected of having celiac disease, the following values should be checked as part of serology:
- The gold standard is the determination of autoantibodies against tissue transglutaminase (tTG / TG2): Transglutaminase antibodies (tTG-Ak / TG2-Ak).
- Total IgA should also be determined routinely, as immunoglobulin A deficiency is more common in people with celiac disease1 - and the immunoglobulin A antibody values obtained are then not meaningful.
- In the case of a total IgA deficiency, IgG antibodies against tissue transglutaminase (tTG-IgG), against endomysium (EMA-IgG) or against deamidated gliadin peptides (dGP-IgG) should be determined.
- HLA typing can used to rule out celiac disease in people who are already on a gluten-free diet or in whom there is a discrepancy between the serological and histological results. It can also be ordered for children with an increased genetic risk.
Which methods are unsuitable for testing for celiac disease?
Due to their insufficient informative value and/or reliability, the following methods are not suitable for diagnosing celiac disease:
- Antibodies against gliadin (AGA)
- Antibodies against wheat germ agglutinin (WGA)
- Saliva and stool tests
- Rapid blood tests
- General IgG tests
When should a small bowel biopsy be performed
In adults with positive celiac disease serology, a small intestine biopsy is indicated to confirm the diagnosis. At least six samples must be taken from different sections of the duodenum including the duodenal bulb and the middle and distal duodenum (two each). The histological changes in these samples are assessed according to the Marsh classification for celiac disease:
- Marsh 0: Healthy small intestinal mucosa and villi
- Marsh I: Increased intraepithelial lymphocytes
- Marsh II: Increased intraepithelial lymphocytes and crypt hyperplasia
- Marsh IIIa to IIIc: Increased intraepithelial lymphocytes and crypt hyperplasia, small intestinal mucosa with partially to completely regressed intestinal villi.
If a biopsy is contraindicated, celiac disease can still be diagnosed if the tTG-IgA concentration is ten times higher than the upper level of normal and EMA-IgA is detected in a second blood sample.
How celiac disease is diagnosed in children
With regard to the diagnosis of celiac disease inchildrenl, paediatric guidelines open up the option of diagnosing celiac disease without a small intestine biopsy under certain conditions:
- TGA IgA values at least ten times above the upper level of normal
- Detection of endomysium IgA antibodies in a second sample
However, a HLA test and the presence of symptoms are no longer mandatory criteria. The advantages and disadvantages of such a celiac disease diagnosis without a small intestine biopsy should be explained by a paediatric gastroenterologist.
When is celiac disease diagnosed?
If the tests confirm the suspicion of celiac disease, a strict gluten-free diet should be prescribed. If the individual's symptoms improve as a result, and a new celiac disease laboratory test shows that the specific celiac disease antibodies respond to the dietary therapy, the diagnosis of celiac disease is confirmed beyond doubt.
What to do if it's not celiac disease?
The wide variety of clinical manifestations lead to an overlap of the symptoms of celiac disease, particularly with other cereal or gluten-related diseases (gluten-related disorders / GRD). Due to this overlap phenomenon, a differential diagnosis in the GRD context is often necessary once celiac disease has been ruled out.
Dr. Schär Institute Newsletter
Bundled gluten-related disorders (GRDs) expertise for your practice: our newsletter keeps you up to date on celiac disease and related topics.
This might also interest you

Practical guide to the diagnosis of wheat allergy
Read more
Irritable bowel syndrome diagnostics in practice
Read moreSources
- Al-Toma A, et al. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United European Gastroenterol J. 2019 Jun;7(5):583-613 , (Accessed 26 Sep 2024)
- Husby S et al. European Society Paediatric Gastroenterology, Hepatology and Nutrition Guidelines for Diagnosing Coeliac Disease 2020. J Pediatr Gastroenterol Nutr. 2020 Jan;70(1):141-156. (Accessed 26/09/2024)
- Felber J et al. Updated S2k guideline coeliac disease of the German Society for Gastroenterology, Digestive and Metabolic Diseases (DGVS), Z Gastroenterol 2022; 60: 790-856. (Accessed 26.09.2024)
