Coeliac disease

Coeliac disease: pathogenesis
It is clear that the autoimmune disease coeliac disease is a reaction to the gluten protein. But what triggers this disease? Coeliac disease is caused by a complex pathology resulting from the interaction of genetic and exogenous factors.
Genetic factors in coeliac disease
A high incidence of coeliac disease of 10-15% among first-degree relatives and around 50-75% among monozygotic twins suggests a genetic contribution to the pathogenesis. An important genetic factor is the human leukocyte antigen system (HLA system), a gene complex whose task is to recognise foreign molecules. Approximately 90% of people with coeliac disease carry the HLA-DQ2 trait, while almost all of the rest express the HLA-DQ8 gene. Although the presence of both gene complexes is necessary for the disease to develop, they are not solely responsible for it. After all, these genes are also found in more than 30-40% of the healthy population.
Exogenous factors in coeliac disease
The only exogenous factor known to date that plays a role in coeliac disease is gluten, a collective term for the storage proteins found in wheat, rye and barley. These proteins have a high proportion of proline and glutamine residues and are referred to as prolamins. Wheat prolamines include gliadins (α, γ and ω gliadins) and glutenins. They cannot be completely broken down by stomach and pancreatic enzymes and trigger the adaptive immune response in coeliac disease.
Research is currently investigating whether and to what extent additional environmental factors – such as infections and the amount of gluten consumed, together with changes in the gut microbiome – play a role in the development of the disease.
Pathophysiology of coeliac disease
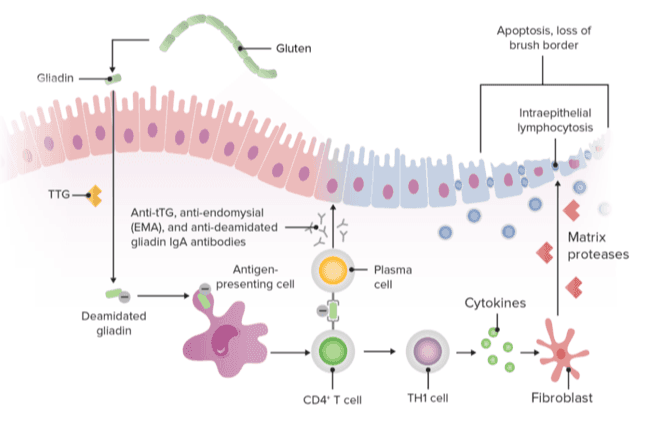
Gluten is usually consumed in large quantities (10-20g/ day) in the normal diet. Some of the gluten peptides are not properly broken down by the stomach and pancreatic enzymes and are absorbed trans-epithelially via the lamina propria (small intestine mucosa).
Transglutaminase (TG2, also known as tissue transglutaminase) deamidateses gluten peptide residues, resulting in better binding to HLA-DQ2 or HLA-DQ8 on antigen-presenting cells (APCs) and potentiating the inflammatory response.
TG2 also causes molecules to link together, leading to the formation of TG2-gluten complexes. This activates:
- T lymphocytes with the release of cytokines and tumour necrosis factor alpha (TNF-alpha).
- B cells with the release of antibodies (anti-tTG and anti-gliadin antibodies).
- Cytotoxic lymphocytes, which interact with intestinal epithelial cells, contributing to tissue destruction and small intestine atrophy.
Dr. Schär Institute Newsletter
Sharing GRD research and expertise for your practice: our newsletter keeps you up to date on coeliac disease and related topics.
You may also be interested in

How to successfully diagnose coeliac disease in practice
Read more
Treating coeliac disease means educating, caring for and motivating people
Read moreSources
- Catassi C, Verdu EF, Bai JC, Lionetti E. Coeliac disease. Lancet. 25 June 2022;399(10344):2413-2426. doi: 10.1016/S0140-6736(22)00794-2. Epub 9 June 2022. PMID: 35691302.
- Gatti S, Rubio-Tapia A, Makharia G, Catassi C. Patient and Community Health Global Burden in a World With More Celiac Disease. Gastroenterology. 2024 Jun;167(1):23-33. doi: 10.1053/j.gastro.2024.01.035. Epub 2024 Feb 1. PMID: 38309629.
- Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet. 2018;391(10115):70-81
- Wieser H. Chemistry of gluten proteins. Food Microbiol 2007; 24: 115–19
- Sollid LM, Qiao S-W, Anderson RP, Gianfrani C, Koning F. Nomenclature and listing of celiac disease relevant gluten T-cell epitopes restricted by HLA-DQ molecules. Immunogenetics 2012; 64: 455–60.
- Pes GM, Bibbò S, Dore MP. Coeliac disease: beyond genetic susceptibility and gluten. A narrative review. Ann Med. 2019 Feb;51(1):1-16. doi: 10.1080/07853890.2019.1569254. Epub 11 March 2019. PMID: 30739507; PMCID: PMC7857446.
- Sharma N, Bhatia S, Chunduri V, Kaur S, Sharma S, Kapoor P, Kumari A, Garg M. Pathogenesis of Celiac Disease and Other Gluten Related Disorders in Wheat and Strategies for Mitigating Them. Front Nutr. 2020 Feb 7;7:6. doi: 10.3389/fnut.2020.00006. PMID: 32118025; PMCID: PMC7020197.
- Iversen R, Sollid LM. The Immunobiology and Pathogenesis of Celiac Disease. Annu Rev Pathol. 2023 Jan 24;18:47-70. doi: 10.1146/annurev-pathmechdis-031521-032634. Epub 6 September 2022. PMID: 36067801.
- Verdelho Machado M. Refractory Celiac Disease: What the Gastroenterologist Should Know. Int J Mol Sci. 2024 Sep 26;25(19):10383. doi: 10.3390/ijms251910383. PMID: 39408713; PMCID: PMC11477276.
