
Self-reported Nonceliac Gluten Sensitivity in Patients with IBS
Brindicci VF, Cristofori F, Franceschini S et al. J Clin Gastroenterol. 2026 Jan 30.
Introduction
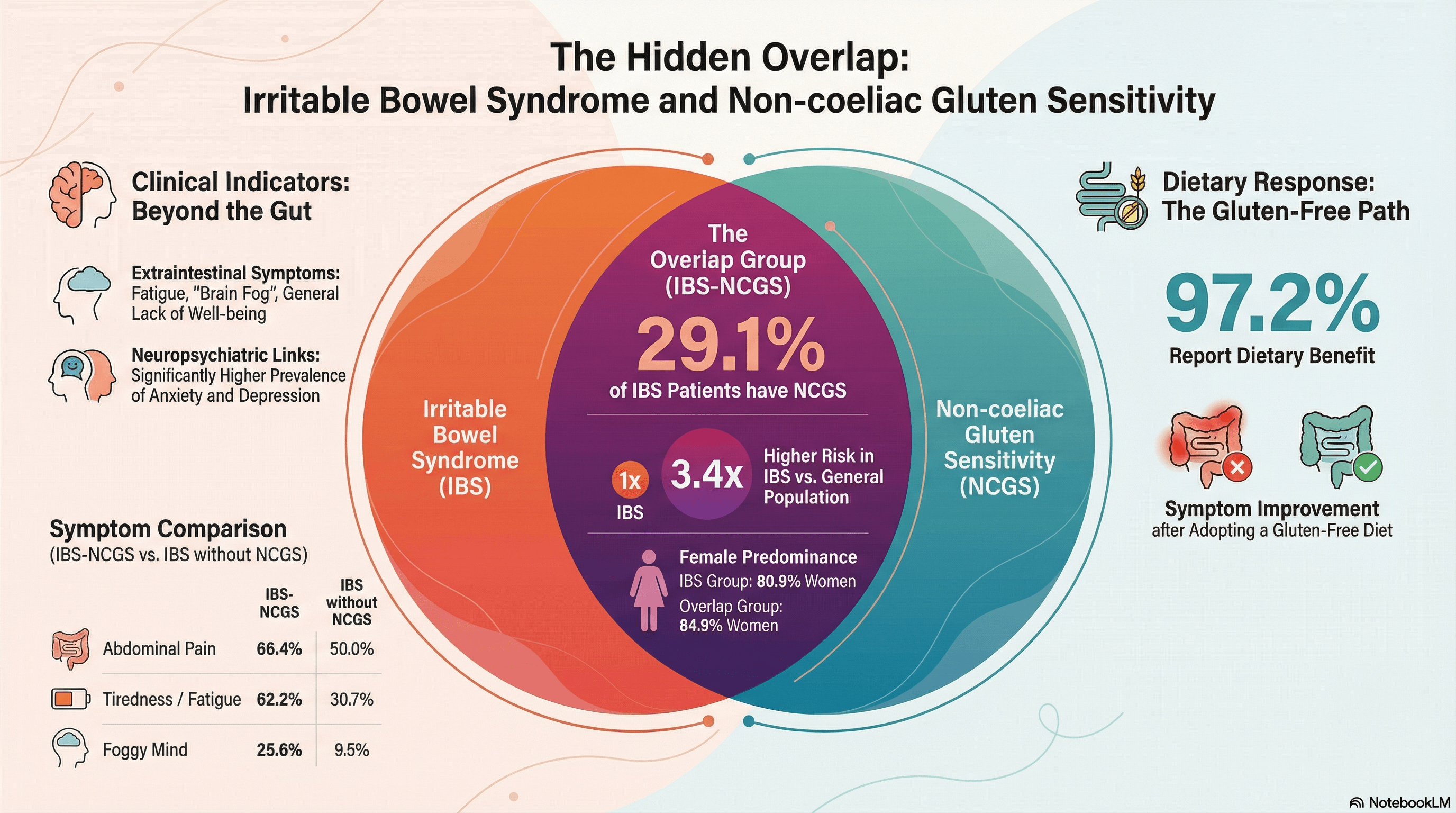
Irritable bowel syndrome (IBS) and Non-coeliac gluten sensitivity (NCGS) are two conditions that share similar gastrointestinal manifestations. Several studies have shown that a subset of IBS patients report symptomatic improvement on a gluten-free diet (in the absence of coeliac disease), giving rise to the hypothesis that a gluten-sensitive IBS subgroup may exist. The precise epidemiology and pathophysiology for this overlap remain poorly defined, with evidence pointing to wheat components other than gluten (such as amylase-trypsin inhibitors and fructans) being responsible. This cross-sectional survey aimed to investigate the prevalence of self-reported NCGS among individuals fulfilling the Rome IV criteria for IBS. The study also sought to investigate potential features that may aid a differential diagnosis in this patient group, and support more personalised, evidence-based dietary recommendations.
Participants and methods
The study was conducted between January and March 2022 across 13 Italian cities, targeting a cohort of young adults aged 18 to 35. Researchers used a modified version of a validated questionnaire, administered outside major shopping centres to ensure a broad population-based sample. The questionnaire was divided into three sections: demographics and medical history, Rome IV criteria for identifying IBS, and gluten-related symptoms and dietary habits.
Results
From 5,108 valid survey responses, the study found that 819 (16%) of participants met the Rome IV criteria for IBS. Within this IBS group, 238 (29.1%) also fulfilled the criteria for NCGS, a significantly higher prevalence than the 8.6% found in the non-IBS population. The researchers noted a clear female predominance, with women making up 80.9% of the IBS group and 84.9% of the IBS-NCGS overlap group.
Key clinical findings included:
- Symptom Profile: While both IBS groups reported gastrointestinal issues like bloating and flatulence, the overlap group was significantly more likely to report** extraintestinal symptoms**, such as fatigue (62.2%), lack of well-being (45.0%), and "foggy mind" (25.6%).
- Mental Health: The IBS-NCGS group had a significantly higher prevalence of neuropsychiatric disorders, specifically** anxiety and depression** (34.0%), compared to those with IBS alone (22.6%).
- Gluten-Free Diet (GFD): Adherence to a GFD was notably higher in the overlap group (60.9%) than in the IBS-only group (40.5%). Furthermore, 97.2% of the overlap group reported symptom improvement on the diet, compared to 70.1% of the IBS-only group.
Discussion
The principal finding-that roughly 30% of IBS patients overlap with NCGS-aligns with previous estimates and suggests that gluten may be a specific trigger for a substantial subset of IBS patients. The authors propose several pathophysiological mechanisms for this overlap, including increased intestinal permeability caused by gliadin-activated zonulin signalling and low-grade inflammation triggered by other wheat components like amylase-trypsin inhibitors (ATIs). The sources suggest that extraintestinal manifestations serve as valuable clinical markers for identifying this overlap. However, the lack of reliable biomarkers means many patients adopt a GFD without a formal diagnosis, which can lead to nutritional imbalances or the misattribution of symptoms that might actually be caused by FODMAPs. While the study's large sample size is a strength, the authors acknowledge the limitations of self-reported data, which reflects subjective experience rather than clinician-confirmed diagnoses.
Conclusion
The study concludes that a significant portion of IBS patients also meet the criteria for NCGS and present with a distinct clinical profile characterised by extraintestinal and neuropsychiatric features. Identifying this specific subgroup is essential for providing personalised treatment strategies. The authors emphasise the urgent need for validated diagnostic tools and biomarkers to distinguish NCGS from other gastrointestinal disorders, which would allow for more precise, evidence-based dietary recommendations and better patient outcomes
Sources
You may also be interested in

A holistic view of the pathogenesis of irritable bowel syndrome (IBS)
Read more
Coeliac disease – the chameleon of gastroenterology
Read more